Tuberculosis (TB), a multisystemic disease with myriad presentations and manifestations, is the most common cause of infectious disease–related mortality worldwide. Although TB rates are decreasing, the disease is becoming more common in many parts of the world. In addition, the prevalence of drug-resistant TB is increasing worldwide.
Causes
Tuberculosis (TB) is caused by a type of bacterium called mycobacterium tuberculosis.
TB is spread when a person with an active TB infection in their lungs coughs or sneezes and someone else inhales the expelled droplets containing TB bacteria.
However, although it is spread in a similar way to cold or flu, TB is not as contagious. You would usually have to spend prolonged periods in close contact with an infected person to catch the infection yourself.
For example, TB infections usually spread between family members who live in the same house. It would be highly unlikely to become infected by sitting next to an infected person on a bus or train.
Not everyone with TB is infectious. Generally, children with TB or people with TB that occurs outside the lungs (extrapulmonary TB) do not spread the infection.
Latent or active TB
Your immune system will usually be able to defeat the bacteria that cause TB. However, in some cases the bacteria infect the body but don't cause any symptoms (latent TB) or the infection will begin to cause symptoms within weeks or months (active TB).
About 10% of people with latent TB develop active TB years after the initial infection. This usually happens when the immune system is weakened, for example during chemotherapy.
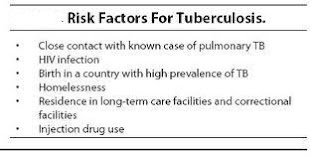
Risk Factors
Anyone can catch TB, but people particularly at risk include:
- those living in environments where the level of existing TB infection is higher than normal
- people with health conditions such as HIV or whose circumstances mean they are less able to fight off a TB infection
Other things that can increase your risk of developing an active TB infection include:
- being in close contact with someone who is infected
- having lived in, travelled to or had visitors from parts of the world where TB is common
- being part of an ethnic group that originated in parts of the world where TB is still common
- having a weakened immune system because of HIV, diabetes or other medical conditions
- having a weakened immune system because of long courses of medication, such as corticosteroids, chemotherapy or tumour necrosis factor blockers (used to treat some types of arthritis)
- being very young or very old – the immune systems of people who are young or elderly tend to be weaker than those of healthy adults
- being in poor health or having a poor diet due to lifestyle and other problems, such as drug misuse, alcohol misuse or homelessness
- living in poor or crowded housing conditions, such as prisons
Signs and Symptoms of TB
People with a latent TB infection don’t have any symptoms, don’t feel sick and cannot infect others. They do, however, test positive to the Mantoux Skin Test. Treating latent TB is important since it can get activated, especially if the immune system is weakened for any reason, including nutritional deficiencies or infection with HIV.
In the case of an active infection, signs and symptoms vary according to the organ that is affected.
In case the lungs are affected, the symptoms are:
- A cough persisting for 2 to 3 weeks and beyond, which is usually worse in the mornings
- Chest pain
- Blood in the sputum (the mucus and saliva produced when coughing or clearing throat)
- Breathlessness
Back pain may be caused by tuberculosis of the spine, and blood in the urine may be caused by tuberculosis in your kidneys.
TB in the brain can cause headaches, a stiff neck, confusion, vomiting, an altered mental state, seizures and other signs and symptoms related to the nerves.
In general, a person with active TB in any organ may have these signs and symptoms:
- Weight loss
- Loss of appetite
- Chills
- Fever
- Sweating in the night time while sleeping, even if the weather is cold.
Diagnosis
Tuberculosis is diagnosed by finding Mycobacterium tuberculosis bacteria in a clinical specimen taken from the patient. While other investigations may strongly suggest tuberculosis as the diagnosis, they cannot confirm it.
A complete medical evaluation for tuberculosis (TB) must include a medical history, a physical examination, a chest X-ray and microbiological examination (of sputum or some other appropriate sample). It may also include a tuberculin skin test, other scans and X-rays, surgical biopsy.
Treatment
Medications are the cornerstone of tuberculosis treatment. But treating TB takes much longer than treating other types of bacterial infections. With tuberculosis, you must take antibiotics for at least six to nine months. The exact drugs and length of treatment depend on your age, overall health, possible drug resistance, the form of TB (latent or active) and the infection's location in the body.
A recent study suggests that a shorter term of treatment — three months instead of nine — with combined medication may be effective in keeping latent TB from becoming active TB. With the shorter course of treatment, people are more likely to take all their medication and the risk of side effects is lessened. More study is needed.
Most common TB drugs
If you have latent tuberculosis, you may need to take just one type of TB drug. Active tuberculosis, particularly if it's a drug-resistant strain, will require several drugs at once. The most common medications used to treat tuberculosis include:
If you have latent tuberculosis, you may need to take just one type of TB drug. Active tuberculosis, particularly if it's a drug-resistant strain, will require several drugs at once. The most common medications used to treat tuberculosis include:
- Isoniazid
- Rifampin (Rifadin, Rimactane)
- Ethambutol (Myambutol)
- Pyrazinamide
There's some evidence that taking vitamin D during tuberculosis treatment enhances some of the effects of the drugs. More study is needed.
Medication side effects
Side effects of TB drugs aren't common but can be serious when they do occur. All tuberculosis medications can be highly toxic to your liver. When taking these medications, call your doctor immediately if you experience any of the following:
Side effects of TB drugs aren't common but can be serious when they do occur. All tuberculosis medications can be highly toxic to your liver. When taking these medications, call your doctor immediately if you experience any of the following:
- Nausea or vomiting
- Loss of appetite
- A yellow color to your skin (jaundice)
- Dark urine
- A fever that lasts three or more days and has no obvious cause
Completing treatment is essential
After a few weeks, you won't be contagious, and you may start to feel better. It might be tempting to stop taking your TB drugs. But it is crucial that you finish the full course of therapy and take the medications exactly as prescribed by your doctor. Stopping treatment too soon or skipping doses can allow the bacteria that are still alive to become resistant to those drugs, leading to TB that is much more dangerous and difficult to treat.
After a few weeks, you won't be contagious, and you may start to feel better. It might be tempting to stop taking your TB drugs. But it is crucial that you finish the full course of therapy and take the medications exactly as prescribed by your doctor. Stopping treatment too soon or skipping doses can allow the bacteria that are still alive to become resistant to those drugs, leading to TB that is much more dangerous and difficult to treat.
To help people stick with their treatment, a program called directly observed therapy (DOT) is sometimes recommended. In this approach, a health care worker administers your medication so that you don't have to remember to take it on your own.
Prevention
Tuberculosis is a preventable and a curable disease if detected and treated early.Some measures of prevention are suggested for those living or travelling to areas and countries that have a high prevalence of the infection.
Tuberculosis vaccine
Bacillus Calmette-Guérin (BCG) vaccination can protect against tuberculosis. The BCG vaccine is given to all infants in countries where the disease is prevalent. In countries where it is less common it is given to those who are at risk.
Before the vaccine is given, the person is given a Mantoux skin test to check for latent tuberculosis. Vaccination is not recommended for people with latent tuberculosis.
Currently, the BCG vaccination is recommended for three main groups of people. One of these are babies born in areas where the rates of tuberculosis is high and those babies with one or more parents or grandparents born in countries with a high rate of tuberculosis. Mantoux skin test will not be required beforehand while giving BCG vaccine to a baby.
Another group that needs BCG vaccine includes children under 16 years of age who have one or more parents or grandparents born in countries with a high rate of tuberculosis and have not been vaccinated as babies. Children under 16 who have been in close contact with someone with tuberculosis or have lived for at least three months in a country with a high rate of tuberculosis are also vaccinated with BCG after getting a Mantoux test.
The third group that requires BCG vaccination are those at high-risk occupations that includes people under 35 years of age whose occupation expose them to tuberculosis infected persons. This includes:-
- health care workers (doctors, nurses and carers)
- laboratory personnel who handle samples of tuberculosis
- veterinary staff and other animal workers, such as abattoir workers who handle animals that may carry tuberculosis
- those working in closed cramped spaces including prisoners, and hostel wardens, staff at orphanages and homes for the homeless etc.
- staff at elderly care homes and refugee homes
- travellers to countries with high rates of tuberculosis who plan to live there for at least 3 months
Prevention of transmission of infection
Those with pulmonary tuberculosis are contagious up to about two to three weeks once their treatment is begun. Earlier these patients were isolated. These days isolation is not practiced but some precautions are important to prevent spread. These include:-
- Isolation from workplaces, schools and college and areas with crowds.
- Covering one’s mouth and nose while coughing or sneezing.
- Adequate and careful disposal of tissues. Usually burning or disposal in sealed plastic bags is recommended.
- Sharing beds and rooms with un-infected persons while sleeping should be avoided.
Please Note
Early detection and treatment of TB is hugely important to stop the spread of this highly contagious disease.Make sure you know the symptoms and risks, so if TB finds a way into your home or workplace, you know what to do.About 1 in 10 latent cases, which present no symptoms, develop into full-blown TB. Knowing who is at risk can be almost as important as knowing what to look for.
If your workplace or environment puts you into one of these high-risk groups, a TB test can be a smart way to prevent developing the disease.
If you, or someone you know, does develop symptoms, it’s important to know what to look for. Most, but not all, infections are located mostly in the lungs, and lead to chestpain,difficulty breathing, and most noticeably, prolonged coughing (often with blood). Those with TB may also experience flu-like symptoms, including chills, aches, fatigue, weight loss, and pallor.
Drug-resistance is rapidly becoming a challenge in the treatment of TB, so quelling outbreaks early is extremely important. Early detection is one of the best steps toward stopping the spread of this preventable disease. Know what to look for and educate those around you, so everyone can breath easy.








No comments:
Post a Comment